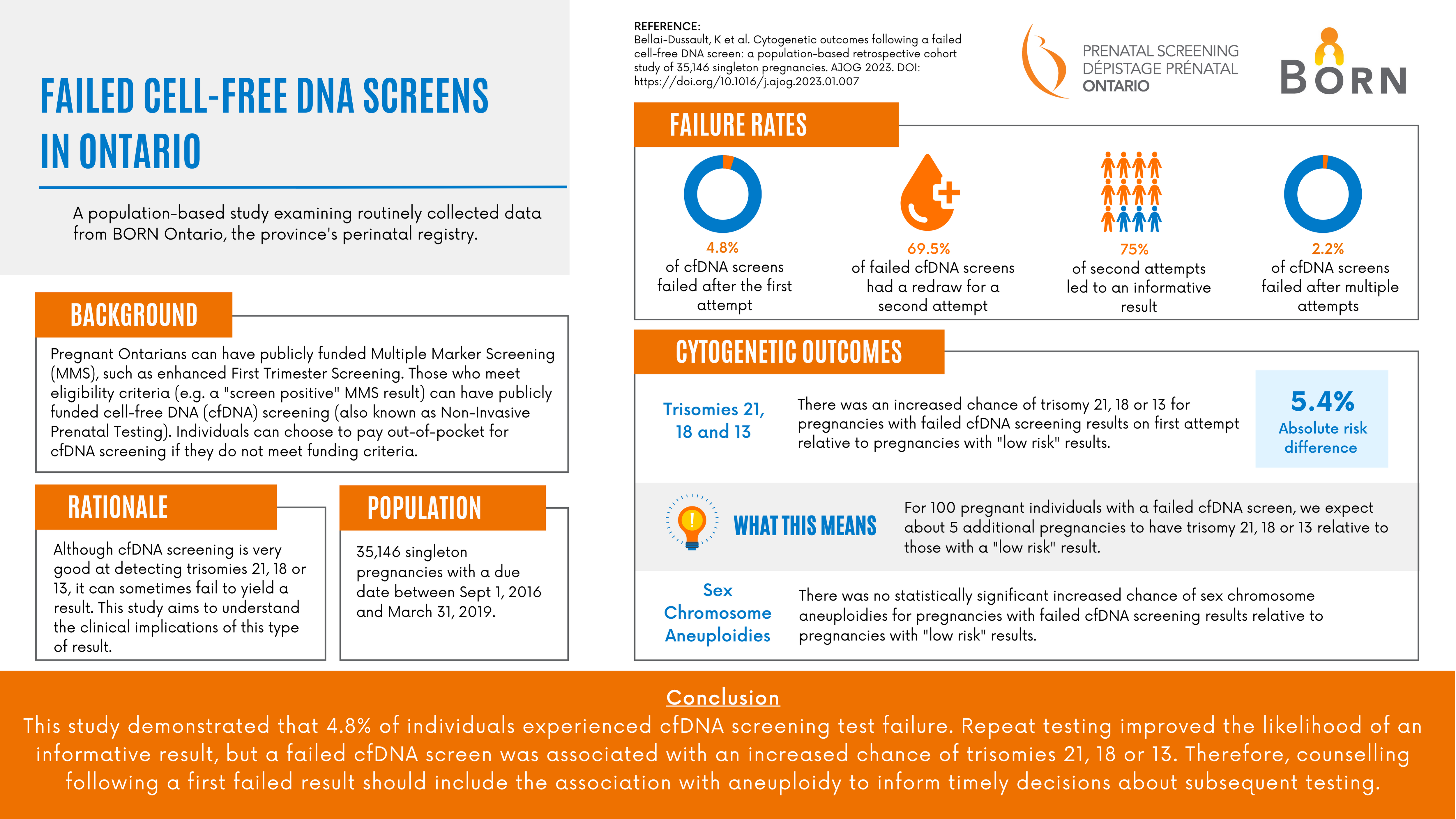
Failed cell-free DNA Screens in Ontario
A population-based study examining routinely collected data from BORN Ontario, the province's perinatal registry.
Background
Pregnant Ontarians can have publicly funded Multiple Marker Screening (MMS), such as enhanced First Trimester Screening. Those who meet eligibility criteria (e.g. a "screen positive" MMS result) can have publicly funded cell-free DNA (cfDNA) screening (also known as Non-Invasive Prenatal Testing). Individuals can choose to pay out-of-pocket for cfDNA screening if they do not meet funding criteria.
Rationale
Although cfDNA screening is very good at detecting trisomies 21, 18 or 13, it can sometimes fail to yield a result. This study aims to understand the clinical implications of this type of result.
Population
35,146 singleton pregnancies with a due date between Sept 1, 2016 and March 31, 2019.
Failure rates
- 4.8% of cell-free DNA screens failed after the first attempt.
- 69.5% of failed cell-free DNA screens had a redraw for a second attempt.
- 75% of second attempts led to an informative result.
- 2.2% of cell-free DNA screens failed after multiple attempts.
Cytogenetic outcomes
Trisomies 21, 18 and 13
- There was an increased chance of trisomy 21, 18 or 13 for pregnancies with failed cfDNA screening results on first attempt relative to pregnancies with "low risk" results.
- The absolute risk difference was 5.4%.
- What this means - For 100 pregnant individuals with a failed cfDNA screen, we expect about 5 additional pregnancies to have trisomy 21, 18 or 13 relative to those with a "low risk" result.
Sex chromosome aneuploidies
There was no statistically significant increased chance of sex chromosome aneuploidies for pregnancies with failed cfDNA screening results relative to pregnancies with "low risk" results.
Conclusion
This study demonstrated that 4.8% of individuals experienced cfDNA screening test failure. Repeat testing improved the likelihood of an informative result, but a failed cfDNA screen was associated with an increased chance of trisomies 21, 18 or 13. Therefore, counselling following a first failed result should include the association with aneuploidy to inform timely decisions about subsequent testing.